In this article we will discuss about the meaning and approaches to design vaccines.
Meaning of Vaccines:
Vaccines may be defined as a preparation of antigenic materials, often combined with adjuvants, that is administered to individuals to induce protective immunity against pathogenic infections.
The antigen may be in the form of live but avirulent microorganisms, killed microorganisms, purified macromolecular antigenic component of a microorganism, or a plasmid that contains a complementary DNA encoding a microbial antigen.
Most commonly used vaccines work by inducing humoral immunity, and attempts to stimulate cell-mediated immune responses by vaccination are ongoing.
ADVERTISEMENTS:
The success of active immunization with vaccines in eradicating infectious disease is dependent on several factors:
1. Vaccines must be able to recognise the important differences between activation of the humoral and cell-mediated immune responses.
2. Vaccines should be able to develop immunological memory.
3. Vaccines should be most effective against infections that are limited to human hosts and are caused by poorly infectious agents whose antigens are relatively invariant.
Approaches to Design Vaccines:
ADVERTISEMENTS:
1. Whole organism vaccine:
Many commonly used vaccines consist of:
(i) Inactivated (killed) or
(ii) Live but attenuated (avirulent) bacterial cells or viral particles.
ADVERTISEMENTS:
(i) Attenuated viral and bacterial vaccines:
In such cases, microbes are treated in such a way that they can no longer cause disease (i.e., their virulence is attenuated or weakened) but retain their capacity for transient growth within an inoculated host.
Attenuation can be achieved by growing the microbes for prolonged periods under abnormal culture conditions. Such process selects only the mutants that can grow better in abnormal culture but are less capable of growth in normal host.
Examples:
Vaccines of tuberculosis was developed from attenuated strains of Mycobacterium bovis called Bacillus Calmette-Guerin (BCG); rubella vaccines from attenuated strain of rubella virus and Sabin polio vaccine developed from attenuated viral strain, are common examples of such vaccines.
Advantages:
(1) Such vaccines result in increased immunogenicity and production of memory cells as a result of which these vaccines often require only a single immunisation and there is no need for repeated boosters.
(2) Such vaccines often induce long- lasting specific immunity, so immunisation in childhood is sufficient for lifelong protection.
Disadvantages:
ADVERTISEMENTS:
(1) The main disadvantages of such vaccines are the possibility to reversion in a virulent form from the attenuated state of the microbes.
(2) Presence of other viruses as contaminants may cause some adverse reactions to the recipients.
(3) Sometimes post-vaccine complications may render a potential vaccine unacceptable.
(ii) Inactivated viral or bacterial vaccines:
A common approach in vaccine production is the use of inactive microbes. In this case, the microbes are inactivated by heat or by chemical means so that they are no longer capable of replication in the host; but the structure of epitopes are maintained. Chemical inactivation by formaldehyde or other alkylating agents are more successful than heat treatment.
Examples:
Whooping cough vaccine, Salk polio vaccine, HIV vaccine are produced by inactivated pathogens.
Advantage:
Killed vaccines induce a predominantly humoral immune responses.
Disadvantages:
(1) Inactivated vaccines often require relatively large and repeated booster doses.
(2) Inactivated whole- organisms may remain associated with some active pathogens that may cause problems.
(3) Inactivated vaccines are less effective than attenuated vaccines.
2. Purified Antigen (Subunit) Vaccines:
Subunits vaccines are composed of specific antigenic macromolecules purified from pathogens and are usually administered with an adjuvant. In general, three forms of such vaccines are in current use:
(i) Polysaccharide vaccine,
(ii) cytotoxin vaccines,
(iii) recombinant antigen vaccines.
(i) Polysaccharide vaccines:
Such vaccines are produced from the hydrophilic polysaccharide capsule of some bacteria. Coating of such capsule with antibodies and/or complement greatly increases the ability of phagocytic cells to phagocytose such pathogens.
Although such polysaccharide vaccines are inefficient inducers of B cell memory. These vaccines often provide long-lived protective immunity, probably because the polysaccharides are not degraded easily and they persist in lymphoid tissues and stimulate specific B cells for long periods.
High affinity antibody responses may be generated against polysaccharide antigens by coupling them to proteins to form conjugate vaccines.
Examples:
The best known polysaccharide vaccines are used against Pneumococcus (causing pneumonia), and Haemophilus influenzae type b (Hib) (causing bacterial meningitis). Such vaccines have the limitation in their inabilities to activate TH cells. However, the Hib vaccine can activate the memory B cells to some degree in absence of a population of memory TH cells, thus establishing its efficacy as a fruitful vaccine.
(ii) Cytotoxin vaccines:
Many bacteria secrete exotoxins that cause many disease symptoms in the hosts. In preparation of cytotoxin vaccines, bacterial exotoxins are first purified and then chemically inactivated to form toxoid. Such toxoids when used as vaccines, these induce production of anti- toxoid antibodies, which can bind to exotoxins and neutralize their effects.
Examples:
Diphtheria and tetanus toxoid vaccines are produced following such methods.
(iii) Recombinant antigen vaccines:
Genes encoding surface antigens of different pathogens like virus, bacteria and protozoa can be cloned and expressed successfully into suitable vectors. Such expressed antigens are then used for vaccine preparation.
Example:
The gene for the major surface antigen of hepatitis B virus (HBs Ag) was cloned in yeast cells. The resulting recombinant yeast cells then were grown in large fermenters; HbsAg were found to accumulate within the yeast cells.
These yeast cells were collected and disrupted by high pressure and recombinant HBs Ag were collected and purified following biochemical techniques. Such recombinant HBs Ag is then used for development of the vaccines.
3. Live Recombinant Vector Vaccines:
A recent approach to vaccine development is to introduce genes encoding microbial antigens into attenuated virus or bacteria (non-cytopathic vectors) and to infect individuals with such vectors. Thus, the vectors serve as sources of the antigen in the inoculated hosts.
One of the great advantages of such vaccines is that the vectors, like other live viruses or bacteria, induce the full complement of immune responses, including strong CTL responses.
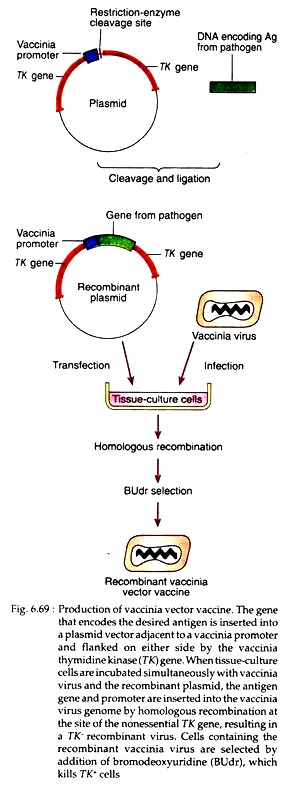
This technique has been used most commonly with vaccinia virus vectors, into which several dozen foreign genes can be inserted without impairing its capacity to infect host cells and replicate. Such genetically engineered vaccinia can express high levels of the inserted gene product, which can then serve as a potent immunogen in the inoculated host (the process for development of such vaccines are shown in Fig. 6.69).
Examples:
Important virus vectors used for recombinant vaccine preparation include canary pox virus, attenuated poliovirus, attenuated strains of Salmonella (for cholera vaccine), BCG strain of Mycobacterium bovis and vaccinia virus (for smallpox vaccine).
A potential problem with viral vectors is that the viruses may infect various host cells, and even though they are not pathogenic, they can produce antigens that stimulate CTL responses, that kill the infected host cells.
4. DNA vaccines:
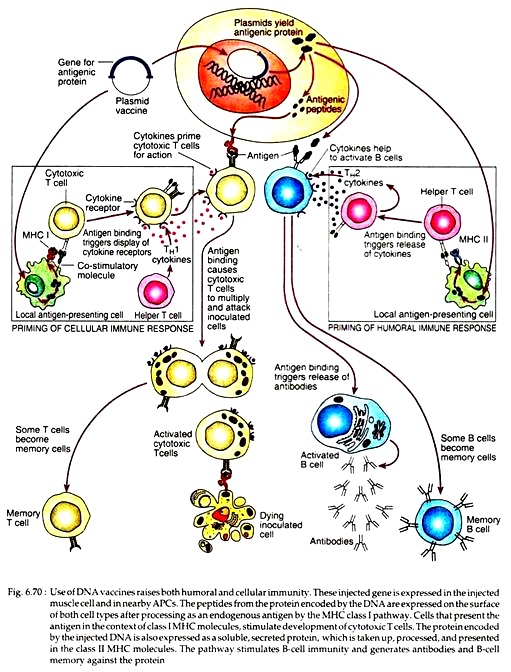
The newest method of vaccination that has developed is the DNA vaccines that offer advantages over many of the existing vaccines. In this vaccination strategy, plasmid DNA encoding antigenic proteins are injected directly into the muscle of the recipient.
The DNA is taken up by muscle cells and the encoded protein antigen is expressed, leading to strong and long-lived humoral and cell-mediated immune responses to the antigen in the host.
The DNA appears either to integrate into the chromosomal DNA or to be maintained for long periods in an episomal form. The viral DNA is expressed not only by the muscle cells but it is likely that APCs, such as dendritic cells are also transfected by the plasmid and the cDNA is transcribed and translated into immunogenic protein that elicits specific response (See Fig. 6.70).
The unique feature of DNA vaccines is that they provide the only approach, other than live viruses, for eliciting strong CTL responses because the DNA-encoded proteins are synthesised in the cytosol of transfected cells.
Furthermore, bacterial plasmids are rich in un-methylated CpG nucleotides and are recognised by a Toll-like receptor (TLR9) on macrophages and other cells, thereby eliciting an innate immune response that enhances adaptive immunity. Therefore, plasmid DNA vaccines are effective even when they are administered without adjuvants.
The practical aspects of such vaccines are also very promising. Refrigeration is not required for the storage of the plasmid DNA, a feature that greatly reduces the cost and complexity of delivery. The same plasmid vector can be custom-tailored to make a variety of proteins, so that the same manufacturing techniques can be used for different DNA vaccines, each encoding an antigen from a different pathogen.
Such vaccines may be applied by coating microscopic gold beads with the plasmid DNA and then be delivered through the skin into the underlying muscle with an air-gun (gene gun), without requiring massive quantities of needles and syringes.
Results to date with DNA vaccines are very promising and at present there are human trials underway with several different DNA vaccines, including those for malaria, AIDS, influenza and herpes virus.
5. Synthetic peptide vaccines:
Synthetic peptides that represent immunodominant T- or B-cell epitopes are being evaluated as vaccines for several diseases. Since peptides are not as immunogenic as proteins, use of conjugates and adjuvants can assist in raising protective immunity to peptides. For the development of such vaccines, the vaccine designers select the peptides that compose immunodominant B-cell epitopes.
Such epitopes can be identified by determining the dominant antibody in the sera of individuals who are recovering from a disease and then testing various synthetic peptides for their ability to react with that antibody with a high affinity.
For example, two linear synthetic peptides representing potential B-cell epitopes of HBs Ag were tested for their binding affinity to pooled antisera from individuals who had recovered from hepatitis B.
In the practical experiment, it was found that a peptide with a cyclical repeats of amino acids 139-147 had a tenfold higher affinity than cyclical repeats of amino acids 124-137. Therefore, the cyclical peptide 139-147 was chosen as a potential one for the synthetic hepatitis B vaccine.
6. Multivalent subunit vaccines:
The above mentioned peptide vaccines are poorly immunogenic and they tend to induce mainly humoral immune responses. To overcome these limitations, a number of innovative techniques are being applied to develop multivalent vaccines that can present multiple copies of a given peptide or a mixture of peptides containing both immunodominant B-cell and T-cell epitopes.
In one approach, solid matrix-antibody antigen (SMAA) complexes are prepared by attaching monoclonal antibodies to particulate solid matrices and then saturating the antibody with the designed antigen. The resulting complexes then can be used as vaccines.
In this way, by attaching different monoclonal antibodies to the solid matrix, it is possible to bind a mixture of peptides or proteins, compositing immunodominant epitopes for both T cells and B cells, to the solid matrix.
Such multivalent complexes can induce vigorous humoral and cell-mediated responses. Furthermore, the particulate nature of such vaccines increases the immunogenicity by facilitating phagocytosis by phagocytic cells.
In another approach, liposomes containing protein antigens are prepared by mixing the proteins with a suspension of phospholipid under conditions that form vesicles bounded by a bilayer. The proteins are incorporated into the bilayer with the hydrophilic residues exposed.
Immunostumulating complexes (ISCOMs) are lipid carriers prepared by mixing protein or peptide antigens with detergent and a glycoside called Quil A. Following these approaches, peptides from various pathogens including influenza virus, hepatitis B virus, measles virus and HIV have been incorporated into liposomes and ISCOMs are currently being assessed as potential vaccines.