Do you want to create an amazing science fair project on mosquitoes. You are in the right place. Read the below given article to get a complete idea on mosquitoes:- 1. Habitat of Mosquitoes 2. Life Cycle of Mosquitoes 3. Biology of Some Common Mosquitoes 4. Habits 5. Role as Vectors 6. Control Measures.
Contents:
- Habitat of Mosquitoes
- Life Cycle of Mosquitoes
- Biology of Some Common Mosquitoes
- Habits of Mosquitoes
- Role of Mosquitoes as Vector
- Mosquitoes Measure Controls
1. Habitat of Mosquitoes:
Mosquitoes constitute the most important group of arthropod-vector from the standpoint of human health. They belong to the family Culicidae of the order Diptera under the class Insecta.
ADVERTISEMENTS:
More than 3,000 species of mosquitoes are found in every part of the world which not only cause great torment through their bites but also serve as efficient vectors for many dreaded human diseases such as malaria, filaria, yellow fever, dengue and encephalitis.
More than a million people die every year from malaria. Other mosquito borne diseases cause incalculable misery, poverty and debilitation. There is considerable concern as to whether mosquitoes can transmit the AIDS virus. At present, transmission has not been demonstrated, but the potential should not be ignored.
2. Life Cycle of Mosquitoes:
Mosquitoes undergo complete metamorphosis with egg, larval, pupal and adult stages, of which larval and pupal stages develop only in water.
i. Eggs:
ADVERTISEMENTS:
Most adult mosquitoes oviposit in water, singly in loosely arranged clusters, each with a float of air cells that provide buoyancy, e.g., Anopheles. In others, such as Culex, eggs are deposited in mass that are vertically arranged in ‘egg-boats’. Species like Aedes and Psorophora lay their eggs singly in moist soil which hatch after a period of drought followed by flooding.
The incubation time varies, ranging from 12 hours to several days in case of eggs in water. The period that elapses from the moment a blood meal is taken until the eggs are laid is called the “gonotrophic cycle”, it is about 48 hours in hot and humid tropical areas.
ii. Larvae:
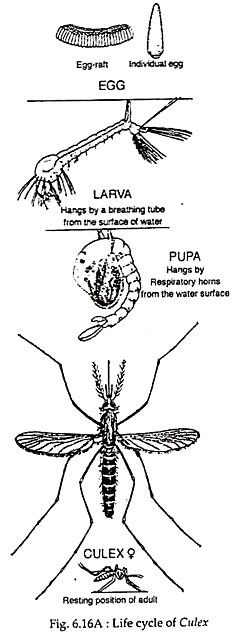
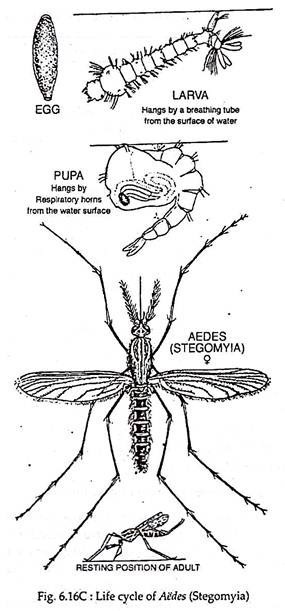
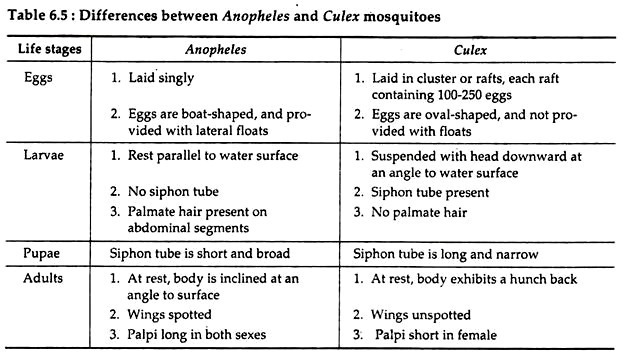
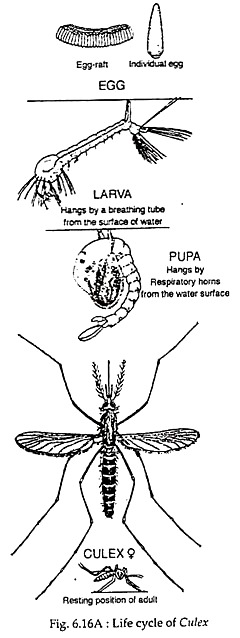
Mosquito-larvae possess an elongated body divisible into head, thorax and abdomen. They possess a breathing siphon or air tube on the posterior segment and mandibulate mouth parts. Larvae of Culex and Aedes remain attached to the water surface by their siphon, but the bodies are directed downward (Fig. 6.16A & C).
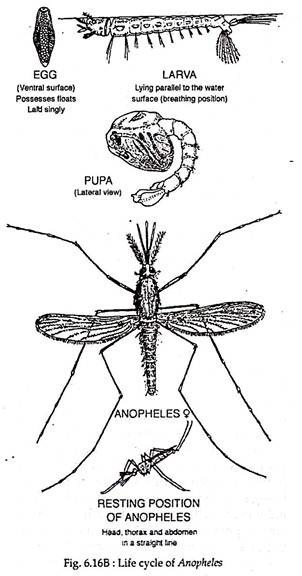
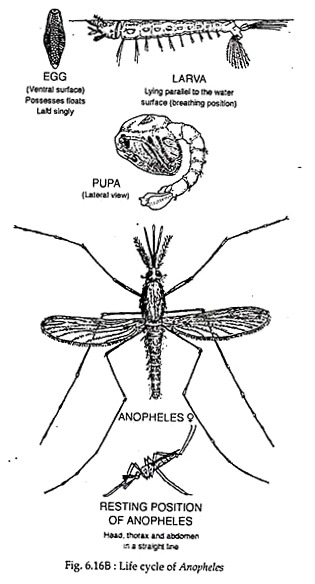
Whereas Anopheles larvae float horizontally (Fig. 6.16B). Majority are free living, filter feeders or browse on microorganisms. Some are predaceous on other insects, including other mosquitoes. The larvae pass through four stages of growth called “instars”, with moulting between each stage.
The first instar is almost microscopic but the ‘ fourth instar measures about 8-15 mm in length. The fourth larval instar after moulting transforms into the pupa. In most cases, the’ larval stage occupies 5-7 days.
iii. Pupae:
The mosquito pupae are comma- shaped in appearance with a large round cephalothorax and a narrow abdomen. A pair of small respiratory tube or trumpet, located dorsally on the cephalothorax, replaces the caudal siphon of the larva. The pupae are extremely active and they flutter up and down in a tumbling action when disturbed.
The pupa represents non-feeding and active tissue re-organisational stage in the life history of the mosquito. The pupation time is short, usually 2-3 days. When fully developed, the skin on the thorax splits and the adult quickly emerges to fly away.
iv. Imagoes/Adults:
Mosquito imagoes or adults are almost similar in morphology. The minute differences in the common species are given in Table 6.5. Adult females live for 4 to 5 months, especially if they undergo a period of hibernation. During hot summer months, females live only about two weeks. Males live about a week, but under optimal conditions, their lifespan may extend to more than a month.
All adult males are vegetarians, feeding on plant juices, but the females are either nectar feeder or blood-suckers.
3. Biology of Some Common Mosquitoes:
ADVERTISEMENTS:
The family Culicidae is composed of two subfamilies – Chaoborinae and Culicinae. About 3,000 species in more than 30 genera are placed in the subfamily Culicinae. From the disease vector stand point Culex, Anopheles and Aedes are the most important genera in our country.
i. Genus Culex:
Culex includes over 480 species from various parts of the world.
Members of this genus can be recognised by some characters:
(i) Palpi short in females, less than one-fifth as long as proboscis.
(ii) Body humpbacked when at rest.
(iii) Tip of abdomen blunt in females, covered with-broad scales.
(vi) Larvae with prominent siphon, armed with numerous tufts of hair.
(vii) Eggs usually deposited in tight floating masses like rafts on surface water (Fig. 6.16a).
Culex fatigans:
C.fatigans is the important vector of filariasis in India. This domestic species is dark brown in colour, breeds freely around human habitation, laying egg rafts in tin cans, tires, cisterns, clogged rain gutters and, in fact, in all types of water collection. It is a strong-winged mosquito and highly anthrophilic. It enters the houses at dusk and reaches maximum density at midnight.
The peak biting time is about midnight. Legs, particularly below the knee, are the preferred biting sites. During day, it may be seen resting indoors on walls, underneath furniture, inside empty pots and in dark corners.
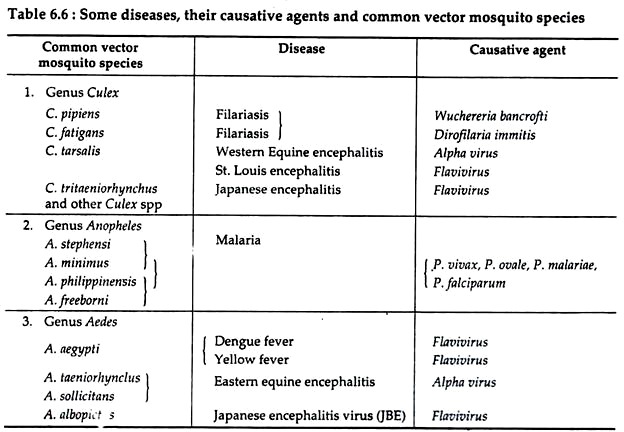
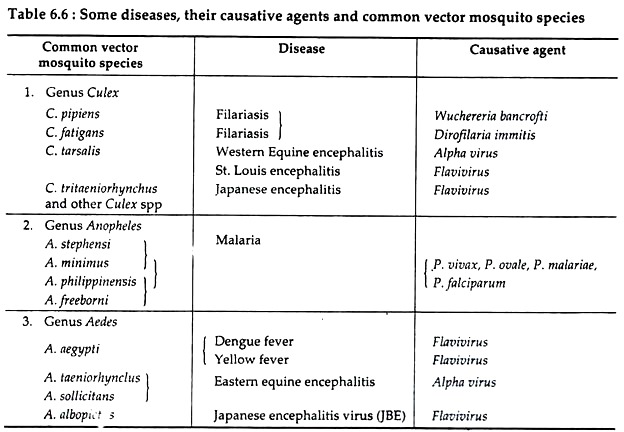
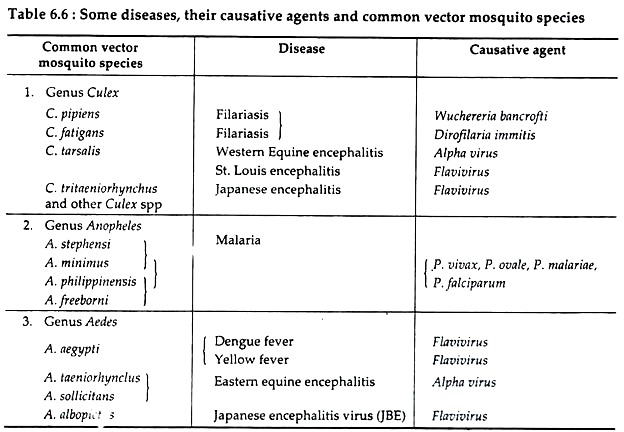
They are important vectors of filarial worms Wuchereria bancrofti and Dirofilaria immitis. They can transmit bird malaria, avian pox, arbovirus encephalitis in addition to Bancroftian filaria. Other important vector species of the genus Culex are Culex tarsalis, the main vector of Western Equine Encephalitis (WEE); and C. pipiens the vector of filariasis (see Table 6.6).
ii. Genus Anopheles:
Some taxonomists place this genus under a separate subfamily Anophelinae.
This genus includes about 400 species which are widely distributed and can be recognised by some characteristics:
(i) Scutellum not lobed.
(ii) Palpi of both sexes usually as long as proboscis.
(iii) Mandibles and maxillae of females well developed and toothed.
(iv) Wings usually spotted or mottled.
(v) Body not humpbacked when at rest but while feeding, body is inclined at a sharp angle from the surface of the host.
(vi) Larvae rest parallel to water surfaces and eggs are laid singly with associated floats.
(vii) Breeding place varies from species to species. Some breed in stagnant, mangrove swamps, others in sunny, partly shaded pools and still others along the edges of trickling streams. A few are free-hole breeders (Fig. 6.16b).
Anopheles spp:
More than 45 species of anopheles mosquitoes have been found in India but only some of them have been incriminated as vectors of malaria. They are A. culicifacies, A. fluviatilis, A. minimum, A. philippinensis, A. stephensi, A. sundaicus and A. leucosphyrus.
They differ in their area of distribution. A. fluviatilis and A. minimum are found in the foothill regions. A. sundaicus and A. stephensi are found in the coastal plain, and A. culicifacies and A. philippinensis are common in the plains.
Female Anopheles spp lay many eggs, depositing them singly on the water. The eggs with lateral floats remain in contact with water to survive. Usually they hatch within 2-6 days and develop through four larval instars in about 2 weeks, followed by three pupal stages. A. stephensi, the most common species of W. Bengal breed in wells, cisterns, roof gutters and any kind of water receptacles.
The females usually bite after midnight. They are the important vector of Plasmodium falciparum, the causative agent of malignant malaria. Besides malaria, Anopheles also transmits bancroftian filariasis in rural settings.
iii. Genus Aedes:
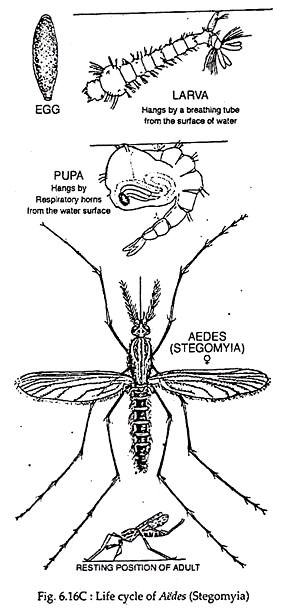
This genus includes about 800 species which are well-represented all over the world.
Members can be identified by the following characters:
(i) Scutellum trilobed.
(ii) Palpi short in females.
(iii) Body humpbacked in resting position.
(iv) Spiracular bristles present.
(v) Abdomen of females pointed non-metallic in colour and bears cerci.
(vi) Claws toothed in females.
(vii) Larvae with short breathing siphons bearing a single pair of posteroventral tufts of hair.
(viii) Eggs are deposited singly on water surface or on mud (Fig. 6.16c).
Aedes aegypti:
This most notorious species of the genus Aedes is the vector of yellow fever. It is widely distributed in India. The adults are characteristically marked with transverse bands of silvery white or yellowish white on the abdomen and with vertical thin stripes on the dorsal surface of the thorax. The legs are also bounded and the tarsi of the last pairs of legs are white.
This species is a tree-breeding mosquito in sylvatic situations, but when associated with human habitation, it breeds freely in containers, cisterns and other water storage units. The females are fearless biters, and they bite chiefly during the day. They do not fly over long distance, usually less than 100 metres.
A. aegypti is the principal vector for the flavivirus causing yellow fever. Another flavivirus disease transmitted by A. aegypti is dengue, also called break bone fever and epidemic haemorrhagic fever. Other important vector species of Aedes mosquitoes are tabulated in Table 6.6.
iv. Genus Mansonia:
Mansonia includes some 50 species, which are widely distributed.
These big sized mosquitoes possess the following characteristics:
(i) Postnotum lacks setae.
(ii) Scutellum trilobed.
(iii) Palpi in females usually one-fourth as long as proboscis or longer.
(iv) Bodies humpbacked when in resting position.
(v) Wing scales large and broad.
The common Indian species are:
M. annulifera, M. uniformis, M. indiana, and M. longipalpis. They breed in ponds and lakes containing aquatic plants or weeds, especially water hyacinth. The eggs are laid in star-shaped clusters on the under surface of the leaves of these aquatic plants. The larvae and pupae are found attached to the rootlets of these plants through which they take air for respiration.
When about to become adult, the pupae come to the surface of water and the fully formed adults emerge and escape. They are the important vectors of microfilariae (Wuchereria bancrofti, Brugia malayi and Dirofilaria immitis) and the yellow fever virus in the tropics.
4. Habits of Mosquitoes:
The habits of mosquitoes have been extensively studied by different entomologists. Here a part of the knowledge of these habits that are essential from the point of view of controlling the mosquitoes as well as for a proper understanding of the part they play in disease transmission will be discussed:
i. Feeding Habits:
The males never bite human for blood meal, they subsist on plant juices. The females on the contrary are haematophagous, require a blood meal once in 2-3 days for the development of eggs. However, some females are anthrophilic, prefer human blood, some prefer animal blood (zoophilic) and some are indifferent in their choice and may feed on both man and animals.
ii. Time of Biting:
In general mosquitoes bite in the evening or in early part of the night, but there are great variations among the species. For example A. stephensi prefer to bite at late night while female A. aegypti is found to bite during day.
iii. Breeding Habits:
Generally, anophelines prefer clean water for breeding; the culicine prefer dirty and polluted water; the aedes prefer artificial collection of water. The mansonia breed in water containing certain types of aquatic vegetation.
iv. Resting Habits:
Mosquitoes obscure themselves during the day in dark and cool corners. Some rest indoors (endophilia) and some outdoors (exophilia). The indoor places include dark corners of houses, upper part of walls, behind pictures and under furnitures. The outdoor places are vegetation shrubs, tree holes, cattle sheds and walls etc.
v. Dispersal:
Mosquitoes do not fly far from their breeding place unless swept by wind currents. The range of flight varies with the species and may range up to 11 kms. Aircrafts and ships have increased the possibility of the dispersal of mosquitoes from country to country. The danger of introduction of mosquitoes infected with yellow fever into India, where the populations have no past experience of the disease is well-recognised.
5. Role of Mosquitoes as Vector:
Mosquitoes are not only vicious pests but also serve as vectors for various pathogenic organisms.
Some major mosquito-transmitted diseases occurring in India with special reference to the role played by vector mosquito species are briefly discussed below:
i. Malaria:
The human malarial parasite Plasmodium requires two types of hosts, an invertebrate (mosquito) and a vertebrate (reptile, bird or mammal). Different species of Anopheles mosquito serve as the suitable vectors of human infecting malarial parasites. In addition to Anopheles, some Culex spp and Aedes spp are the major vectors for avian malaria.
When an infected mosquito takes blood from a vertebrate, it injects saliva containing tiny, elongated sporozoites into the blood stream. Thus it transmits the pathogen to a definitive host. After entry in man, the sporozoites first undergo exoerythrocytic schizogony in liver and then erythrocytic schizogony in RBC where gametocytes are produced.
Erythrocytes containing gametocytes when imbibed by susceptible female Anopheles, the parasites get transferred to its intermediate hosts. In the stomach of mosquito, the formation of macro-and microgametes and fertilization do occur. The resultant diploid zygotes soon become a motile ookinete that penetrates the peritrophic membrane in the mosquito’s gut and migrates to the haemocoel side of the gut.
There it first transforms into oocyst. Within oocyst, many sporoblasts are formed which in turn develop into sporozoites that break out of oocyst into haemocoel and migrate throughout- the mosquito’s body. On contacting the salivary gland, sporozoites enter its channels from where these can be injected into a new host at the time of next feeding.
Once infected, a mosquito remains infective for life, capable of transmitting malaria to every susceptible vertebrate it bites. Anopheles spp thus are good vectors for human malaria, live long enough to feed on human blood repeatedly. In this way, mosquito, specially Anopheles spp act as vector for human malarial parasites.
ii. Filaria:
Filariasis in human is caused mainly by nematode worm Wuchereria bancrofti (Bancrofti filaria) and Brugia malayi (Malayan filariasis). Unlike the malarial parasite, filarial worms show little specificity in regard to mosquito hosts. The parasites can utilise Culex spp, Aedes spp, Mansonia spp, Anopheles spp and Psorophora spp as vectors equally well.
Adult W. bancrofti lives in the major lymphatic ducts of human where the ovoviviparous female worms produce thousands of juveniles, known as microfilariae. Most microfilariae then sweep into peripheral blood stream at certain time. Mosquitoes ingest microfilariae along with their blood meal when biting human.
Ingested microfilariae pass through mosquito gut and develop to filariform J3 through first and second stage juveniles (J1 and J2). The infective J3 migrates throughout the haemocoel, eventually reach the labium or proboscis sheath from which they enter the definitive host (human) through the skin wound made by the mosquito.
After migrations through the peripheral lymphatics, the worm settle in the large lymph vessels where they mature. In this way infective mosquitoes transmit filarial parasite to humans. It has been determined that the infection of mosquitoes can only occur if 15 or more microfilariae are present in every 20 mm3 of blood. If there are 100 or more microfilariae in every 20 mm3 of blood, the mosquito is commonly killed.
iii. Dengue:
Dengue is an acute viral infection, caused by at least 4 serotypes (1, 2, 3 and 4) of dengue viruses which are arbo-viruses. Aedes aegypti, A. albopictus, A, polynesiensis are the main vector mosquito species of dengue (Table 6.6). The infection may be asymptomatic or may lead to (a) “classical” dengue fever or (b) dengue haemorrhagic fever with or without shock.
Dengue fever can occur epidemically or endemically. Epidemics may be explosive and often start, during the rainy season when the breeding of the vector mosquitoes is generally abundant. Temperature also plays an important role in the transmission of dengue viruses by mosquitoes.
Mosquitoes kept at 26°C fail to transmit DEN-2 virus. Dengue viruses are now endemic in many countries like India, Burma (Myanmar), Bangladesh, Sri Lanka, Thailand and Malaysia.
The reservoir of dengue infection is both man (no other vertebrate) and mosquito. The transmission cycle is “man-mosquito-man”. The mosquito becomes infective by feeding on a patient from the day before onset to the 5th day (viraemia stage) of illness.
After an extrinsic incubation period of 8 to 14 days, the mosquito becomes infective and is also able to transmit the infection. Once the mosquito becomes infective it remains so for life, but never pass to next generation. However, trans- ovarian transmission of dengue virus has been demonstrated in laboratory.
Following entry in mosquito body, only a few viruses invade its tissues, where the viruses undergo proliferation. The viruses then go to the salivary gland from where they enter the host body at the time of biting. Infection with one dengue serotype give immunity against that particular serotype and partial protection against others.
All ages and both sexes are susceptible to dengue fever. In man, the illness is characterised by an incubation period of 3 to 10 days (commonly 5-6 days). The onset is sudden with chills and high fever, intense headache, muscle and joint pains. Within 24 hours retro-orbital pain and photophobia develop.
Other common symptoms include extreme weakness, anorexia, constipation, colicky pain, abdominal tenderness, dragging pain in inguinal region, sore throat etc. Skin eruption appears in 80% of cases during the remission or during second febrile phase, which may last for 1-2 days.
Fever lasts for about 5 days, rarely more than 7 days after which recovery is usually complete although convalescence may be protracted. The fatality case is low.
Dengue haemorrhagic fever (DHF) is a severe form of dengue fever caused by infection with more than one dengue virus. The severe illness is thought to be due to double infection with dengue viruses – the first infection probably sensitize the patient, while the second appears to produce an immunological catastrophy. It is transmitted by A. aegypti.
Following an incubation period of 4-6 days, the illness commonly begins abruptly with high fever accompanied by facial flushing and headache, anorexia, vomiting, tenderness at the right costal margin. The major pathophysiologic changes that determine the severity of this disease and differentiate it from dengue fever are plasma leakage and abnormal haemostasis and thrombocytopenia.
6. Mosquito Control Measures:
While there are many methods of mosquito control, experts now recommend an “integrated approach”, that is an approach which avoids excessive use of any one method, e.g., insecticides.
Simultaneously such approach tries to combine one or more methods with a view to obtain maximum results with minimum inputs and also prevent environmental pollution with toxic chemicals and development of insecticide resistance.
The various methods of mosquito control may be classified as follows:
1. Anti-larval measures:
(a) Environmental control
(b) Chemical control
(c) Biological control
2. Anti-adult measures:
(a) Residual sprays
(b) Space sprays
(c) Genetic control
3. Protection against mosquito bites:
(a) Mosquito net
(b) Screening
(c) Repellents
i. Anti-Larval Measures:
(a) Environmental control:
“Source reduction” is the most important environmental control measure that includes minor engineering methods such as filling, leveling and drainage of breeding places, and water management, i.e., intermittent irrigation to breeding field. Source reduction needs accurate knowledge of the breeding habits of different mosquitoes.
For Culex, abolition of domestic and peridomestic sources of breeding such as cesspools, open ditches and arrangement for disposal of sewage and waste water are required. In case of Aedes larva control, the environment should be cleaned up and got rid of water holding containers like discarded tins, empty pots, broken bottles, coconut shells and similar artificial collection of water.
If Anopheles mosquitoes are a problem, their breeding places should be abolished by engineering measures such as filling and drainage. For Mansonia larvae control, the aquatic plants to which the larvae attach themselves should be removed or destroyed by herbicides.
(b) Chemical control:
The most commonly used larvicides (chemicals that kill the larvae) are (i) mineral oil, (ii) Paris green, and (iii) synthetic insecticides. Most commonly used mineral oils are the diesel oil, fuel oil, kerosene and various fractions of crude oils.
When applied on water, oil spreads and form a thin film which cuts off the air supply to the mosquito larvae and pupae. It is customary to apply oil once a week on all breeding places. However, oil has some disadvantages, it renders water unfit for drinking and it kills fishes and other aquatic animals also.
Paris green or copper acetoarsenite is an emerald green, micro-crystalline powder that also contains 50 per cent arsenious oxide. It is insoluble in water and acts as a stomach poison. Thus, to be effective it must be ingested by the larvae. Paris green mainly kills the Anopheles larvae because they are surface-feeders.
It is applied by mixing 2 kg of Paris green and 98 kg of a dilutant such as soap-stone powder or slaked lime in a “rotary mixer”. The recommended dose is 1 kg of actual paris green per hectare of water surface. This dose is not harmful to fish, man or other domestic animals.
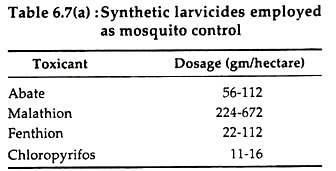
Common synthetic mosquito-larvicides include several organophosphorous compounds like fenthion, chloropyrifos and abate. These are hydrolysed quickly in water and less toxic to other animals. Dosages of these compounds are given in Table 6.7(a).
(c) Biological control:
In recent years, there has been a revival of interest in the biological control of mosquito through the use of fish. A wide range of small fishes, feed readily on mosquito larvae. The most common are the Gambusia affinis and Lebister reticulate.
These fishes (larvicidal fishes) can be cultured in burrow pits, sewage oxidation ponds, cisterns and farm ponds. However, it is now recognised that biological control can be effective only when used in conjunction with other methods.
ii. Anti-Adults Measures:
(a) Residual sprays:
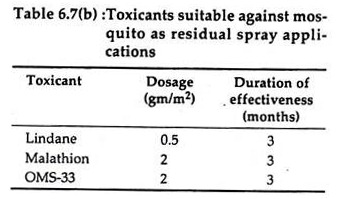
Adult mosquitoes are most commonly controlled by spraying houses with residual insecticides like malathion, propoxur (OMS-33) and gamma- HCH (lindane). Dosage and average duration of the effectiveness are given below (Table 6.7b):
Resistance to insecticides has become common among mosquitoes, especially after several years of exposure. So it is essential that periodic tests should be made to determine the susceptibility of different species to the various insecticides, so that only potent insecticides can be used.
(b) Space sprays:
Space sprays are applied into the atmosphere in the form of a mist or fog to kill insects. The common space sprays used to kill mosquito are pyrethrin, an extract of pyrethrum flowers which acts as a nerve poison and kills mosquito instantly on mere contact. It is effective in reducing the number of mosquitoes but the reduction is only temporary since it has no residual action.
Re-infestation from outside sources generally occurs within a short time. For ultra-low volume (ULV) space spraying, new equipment has been developed. The most extensively used insecticides are malathion and fenitrothion for ULV fogging.
(c) Genetic control:
Control of mosquitoes by genetic methods such as sterile male technique, cytoplasmic incompatibility, chromosomal translocation, sex distortion, and gene replacement has been explored. Genetic controls have several advantages over chemical methods, being cheaper and more potential and above all not subject to vector resistance. However, in our country, the genetic control is still in “research phase”.
iii. Protection against Mosquito Bite:
(a) Mosquito net:
The mosquito net offers protection against mosquito bite during sleep. There should not be a single hole or vent in the net. The size of the openings in the net is of utmost importance – the size should not exceed 0.0475 inch in diameter.
(b) Screening:
Screening of building with copper or bronze gauze having 16 meshes to the inch is recommended. The aperture should not be larger than 0.0475 inch. Screening of building is costly, but gives excellent results.
(c) Repellent:
Diethyltoluamide (Det) has been found to be an outstanding all- purpose repellent. It has been found to remain active against C.fatigans for 18-20 hours. There are others which are also effective: indalone, dimethyl phthalate, dimethyl carbate, ethyl hexanediol etc. Repellents are used mainly for application on the skin or as mats, coils. Their chief advantage is acurate duration of protection.