The hormones are released in very small quantities, yet they cause wide spread responses in cells or tissues all over the body. These responses can be quite specific and selective in different cells.
All vertebrate hormones belong to one of the four chemical groups:
(i) Hormones such as adrenaline and thyroid hormone are small molecules derived from amino acid tyrosine.
(ii) Hormones such as vasopressin and oxytocin are short peptides.
ADVERTISEMENTS:
(iii) Hormones such as insulin and glucagon are longer polypeptide chains.
(iv) Hormones such as testosterone and estrogen are steroid.
All hormones do not act in the same way. Catecholamines (epinephrine and norepinephrine), peptide and polypeptide (protein) are not liquid soluble, therefore, they cannot enter their target cells through the bilipid layer of plasma membrane (cell membrane). Instead, these water soluble hormones interact with a surface receptor, usually a glycoprotein, and, thus, initiate a change of events within it. The hormone insulin provides a well-studied example of how this happens.
The molecular mechanism of hormone action is described under two separate headings:
ADVERTISEMENTS:
1. Mode of hormone action through the extracellular receptors and
2. Mode of hormone action through the intracellular receptors.
1. Mode of Hormone Action through Extracellular Receptors:
The molecules of amino acid derivatives, peptides or polypeptides (protein) hormones bind to specific receptor molecules located on the plasma membrane. The hormone-receptor complex causes the release of an enzyme adenylate cyclase from the receptor site.
ADVERTISEMENTS:
This enzyme forms cyclic adenosine monophosphate (cAMP) from ATP of the cell. The cAMP activates the existing enzyme system of the cell. This accelerates the biochemical reactions in the cell. The hormone is called the first messenger and the cAMP is termed the second messenger.
A detailed description of mode of hormone action through the extracellular receptors is given below:
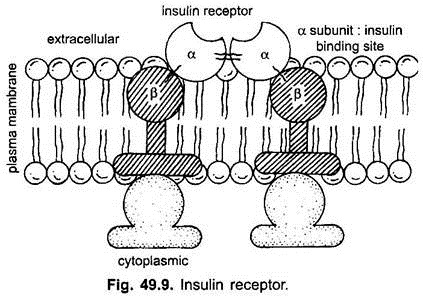
The hormone insulin provides a well-studied example to explain the mode of hormone action through the extracellular receptors. The membrane bound receptors of insulin is a protein consisting of four subunits- two α-subunits and two β-subunits. The two α-subunits protrude out from the plasma membrane (cell membrane) and bind insulin. The two β-subunits protrude into the cytoplasm of the cell. These receptors are usually less than 100 in most cells in our body but may be more than 1,00,000 in some liver cells.
(i) Binding to the Receptor:
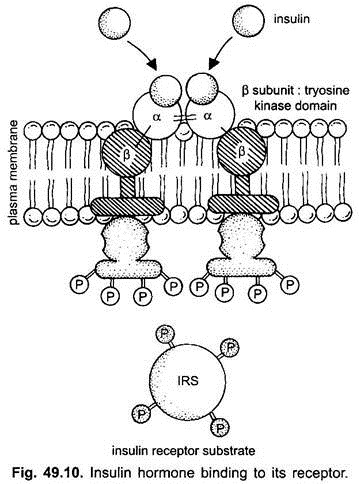
Binding of insulin to the outer α-subunits of the receptor causes a structural change in the β-subunits, which is also an enzyme, a tyrosine kinase. The activated β-subunits add phosphate groups of specific tyrosine residues located in cytoplasmic domain of the receptor, as well as a variety of insulin receptor substrates.
(ii) Second Messengers-The Mediator:
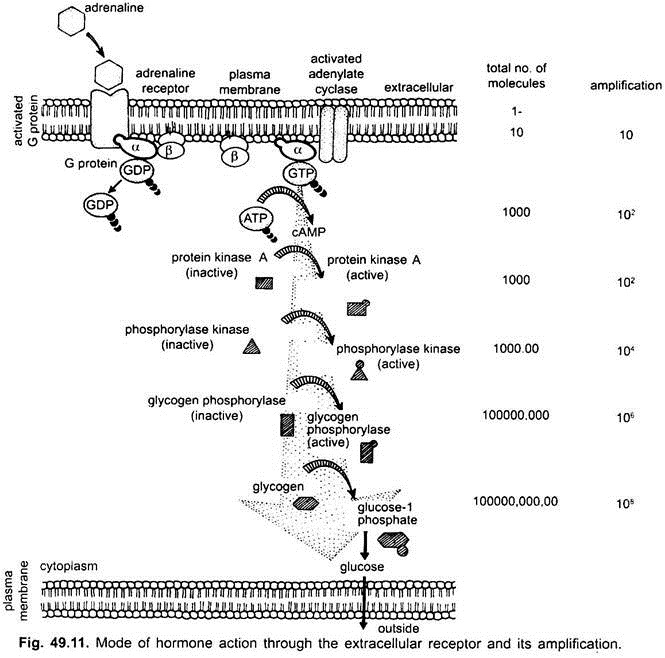
A second example which is widely used in hormonal control of cell function is through adenylate cyclase. The hormone-receptor complex does not directly stimulate adenylate cyclase. It is done through a transducer G-protein. Alfred Gilmans has shown that the G-protein is a peripheral membrane protein consisting of α, β and γ subunits. It interconverts between a GDP form and a GTP form.
In muscle or liver cells, the hormones such as adrenaline bind receptor to form the hormone-receptor complex in the plasma membrane. The hormone-receptor complex induces the release of GDP from the G-protein. The α-subunit bearing GTP dissociates from βγ subunit of G-protein. The activated βγ-subunit of G-protein activates adenylate cyclase. The activated adenylate cyclase catalyses the formation of cAMP from ATP.
G-protein activates enzyme phosphodiesterase. This enzyme makes phosphatidylinositol 4,5 biphosphate (PIP2) into a pair of mediators: inositoltriphosphate (IP3) and diacylglycerol (DG). IP3 and DG are examples of second messengers. IP3 is water-soluble, therefore, diffuses into cytoplasm to release another messenger Ca2+ ions from intracellular endoplasmic reticulum activating many calcium-mediated processes.
While DG remains in the plasma membrane where it activates an enzyme protein kinase C, which in turn, activates many other enzymes such as pyruvate dehydrogenase to bring about the physiological effects.
(iii) Amplification of Signal:
The increased level of cAMP activates the enzyme protein kinase A. Activated protein kinase A activates the enzyme phosphorylase kinase. Each molecule of protein kinase activates about 100 molecules of enzyme, phosphorylase kinase and soon. As a result, a single molecule of adrenaline releases as many as 100 million molecules of glucose within only 1 or 2 minutes. However, a very small quantity of hormone is needed.
In a few instances, cyclic guanosine monophosphate (cGMP) which is only slightly different from cAMP acts in similar manner as a “second messenger”.
(iv) Antagonistic Effect:
The effect of hormones which act against each other are called antagonistic effect. Many body cells use more than one second messenger. In heart cells, cAMP acts as a second messenger that increases muscle cell contraction in response to adrenaline, while cyclic guanosine monophosphate cGMP acts as another second messenger which decreases muscle contraction in response to acetylcholine.
Thus, the sympathetic and parasympathetic nervous systems achieve antagonistic effect on heartbeat. Another example of antagonistic effect is insulin and glucagon. Insulin lowers blood sugar level, while glucagon raises blood sugar level.
(v) Synergistic Effect:
When two or more hormones complement each other’s actions and they are needed for full expression of the hormone effects, are called synergistic effects. For example, the production, secretion and ejection of milk by mammary glands require the synergistic effects of estrogens, progesterone, prolactin and oxytocin hormones.
Thus, it is evident from the above description that cAMP is not the only second messenger utilised by different hormones. Besides cAMP, certain other intracellular second messengers, are cyclic guanosine monophosphate (cGMP), diacylglycerol (DG), inositol triphosphate (IP3) and Ca2+.
2. Mode of Hormone Action through Intracellular Receptors:
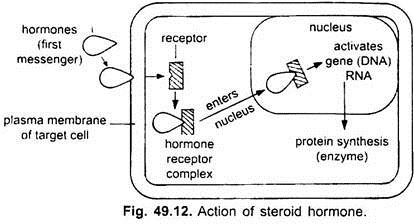
Steroid and thyroid hormones are lipid soluble and easily pass through the plasma membrane (cell membrane) of a target cell into the cytoplasm. In the cytoplasm, they bind to specific intracellular receptor proteins forming a hormone-receptor complex that enters the nucleus. In the nucleus, the hormone-receptor complex binds to specific regulatory sites on the chromosomes and activates certain genes (DNA).
The activated gene transcribes mRNA which directs the synthesis of proteins and usually enzymes in the cytoplasm. The enzymes promote the metabolic reactions in the cell. The actions of lipid-soluble hormones are slower and last longer than the actions of water-soluble hormones. These cause physiological responses that are characteristic of the steroid hormones.
Role of Hormones as Messengers and Regulators:
(Role of Hormones in Homeostasis):
1. Hormones as Messengers [Hypothalamo-Hypophysial (Pituitary) Axis]:
Hypothalamus is a part of the forebrain. Its hypothalamic nuclei-masses of gray matter containing neurons, are located in the white matter in the floor of the third ventricle of the brain. The neurons (neurosecretory cells) of hypothalamic nuclei secrete some hormones called neurohormones (releasing hormones or releasing factors) into the blood.
The neurohormones are carried to the anterior lobe of the pituitary gland (hypophysis), by a pair of hypophysial portal veins (Fig. 49.12). In the pituitary gland (hypophysis) the neurohormones stimulate it to release various hormones. Hence, the neurohormones are also called “releasing hormones or releasing factors”.
2. Hormones as Regulators (Feedback Control):
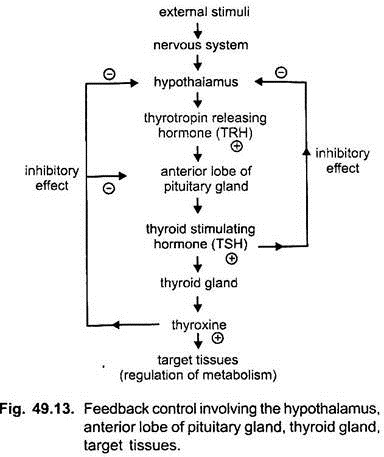
Homeostasis means maintenance of static or constant conditions in the internal environment of the body. Essentially all the organs and tissues of body perform functions. Hormones help to regulate cellular functions. When the secretion of hormones is under the control of factors or other hormones it is called feedback control. The regulation of secretion of thyroxine from the thyroid gland is an example of such feedback control mechanism. Feedback control is of two types.
(i) Positive Feedback Control:
If the level of thyroxine is less than the normal limits in the blood, thyroxine level stimulates the hypothalamus to secrete more of TRH which results in the increased secretion of thyroxine. Such regulatory effect is called positive feedback control.
(ii) Negative Feedback Control:
The thyroxine releasing hormone (TRH) from the hypothalamus stimulates the anterior lobe of the pituitary gland to secrete the thyroid stimulating hormone (TSH). The TSH in turn stimulates the thyroid gland to secrete thyroxine. A high level of thyroxine in the blood exerts an inhibitory effect on hypothalamus in such a way that less of TRH and TSH is produced respectively. This eventually results a decrease in thyroxine. This is called negative feedback control.